DVA claims: Troubleshooting and Frequently Asked Questions
Fill out the HW027 form to register for Online Claiming. Use reason codes to troubleshoot DVA claim issues. For cancellations, contact DVA directly. Ensure correct service type for successful claims.
Important
- You must fill out your HW027 form to register for Online Claiming. If you or any providers that submit claims through your account have not filled out this form previously please do so immediately. Details on how to fill out the form and submit it to Medicare can be found here. Please keep Question 3 on the form blank.
- The requirement for a referral when submitting DVA claims depends on the type of service and the color of the patient’s DVA card. When both the servicing provider and the referring provider are valid, Zanda will process the claim without interruption. To help prevent errors, please ensure all information is entered accurately before submitting your claim.
Sometimes you may get a response from DVA other than ‘Referred’ which generally means that the claim has been unsuccessful. Usually, these responses will be accompanied by a reason code (ie. ‘257’). You can use these codes to discern why the claim wasn’t successful and, in some circumstances, what changes you need to make in order for the claim to go through successfully when resubmitted.
You can find an explanation of each of these codes on the Services Australia website.
Hint 💡
You can press Ctrl + F (Command ⌘ + F on a Mac) on your keyboard to search the page for a specific item code - just input the reason code’s number and hit enter, your browser should then take you to that reason code.
Cancelling a DVA Claim: DVA claims can't be cancelled through Zanda once submitted. To cancel a DVA claim, you'll need to contact DVA directly to request cancellation of the claim. You can contact DVA on their Provider Invoicing and Billing Enquiries number here: 1800 552 580
Which type of claim should I submit?
Generally speaking, most users will submit DVA Allied Health claims, though General Practitioners, those providing Pathology Services, or Specialists will need to use the DVA Medical/Paperless claiming method.
The service type for the Provider is not consistent with the type of claim being submitted. Please click “Edit Provider” > Insurers > Edit the insurance and select a service type that matches the type of claim being submitted
The service type selected for the provider's insurance (Medicare or DVA) will need to be updated. The service type includes the type of claim that it can be used for in brackets after the service type name as shown in the list of service types below:
- General Practitioner (Medicare / DVA Medical)
- Specialist & Allied Health (Medicare / DVA Medical)
- Pathology (DVA Medical)
- Community Nursing (DVA Allied Health)
- Speech Pathology (DVA Allied Health)
- Allied (DVA Allied Health)
- Psychology (DVA Allied Health)
If you are submitting a Patient Claim or Bulk Bill, then you will need to choose a service type with the (Medicare / DVA Medical) label (i.e. General Practitioner or Specialist & Allied Health).
If you are submitting a DVA Medical/Paperless claim you will need to choose a service type with the (Medicare / DVA Medical) or (DVA Medical) label. (i.e. General Practitioner, Specialist & Allied Health, or Pathology)
If you are submitting a DVA Allied Health claim you will need to choose a service type with the (DVA Allied Health) label (i.e. Community Nursing, Speech Pathology, Allied, or Psychology).
DVA Error Codes
DVA claims can be rejected with either a 4 digit return code which will come up as soon as you attempt to submit the claim, or a 3 digit reason code if the claim was submitted but then rejected after being assessed. You can check these by going to Tools > Medicare, clicking on the Claim ID for any Rejected claims or Referred claims where the paid column is showing $0.00. Any return codes for Rejected claims will be shown on the top right of the claim overview page, and the return codes for claims that were rejected after being assessed will be found in the Processing Report on the lower right of the page.
Both the 4 digit return codes and 3 digit reason codes for rejected claims typically have an error message alongside them advising what the issue is, and you'll then be able to fix any issues on the claim and resubmit it. You can find a full list of both return codes and reason codes here on Service Australia's website if no error message is shown:
We've included some troubleshooting steps for more common errors here below as well.
9202: Invalid value of [N] supplied for referral period code. The value supplied must be S (Standard). Error located in medical event 01.
- If submitting a DVA Allied claim where a referral is being used, then the referral period must be a Standard period of either 3 or 12 months. This error is being returned because the referral does not have a standard referral period of 3 or 12 months. Please edit the referral linked to the invoice being claimed and update the referral End date to reflect the referral period.
9202 : Invalid Value of [I] supplied for referral period code. The value supplied must be [S] (standard). Error located in medical event 1.
- This code/error refers to an (I) 'Indefinite' referral period entered under the Profile → Referrals which is not accepted for this particular claimant and/or claim. The Referral period should be set to (S) Standard (12 months from a GP and 3 months from a Specialist) or if Referral period set to Non standard, the period should be specified in the Service Text.
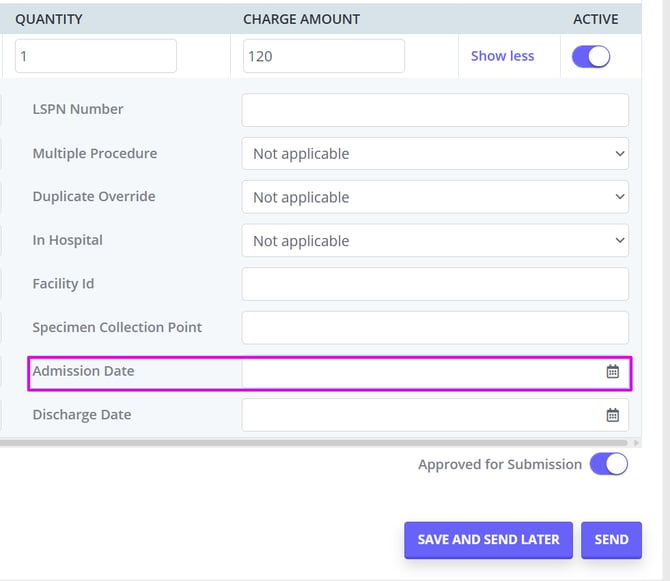
2030: Additional information required. If Service Type Code is set to F (Community Nursing) then Admission Date must be supplied. Error located in Medical Event {m}, Service {s}.
The Admission Date is the date the patient was admitted to hospital. It must be supplied to Medicare for Community Nursing service type. Note: For DVA community nursing, this is the admission date to the nursing service.
To add the Admission Date, generate the DVA claim and click on Show More at the bottom right. Enter the Admission Date as required.
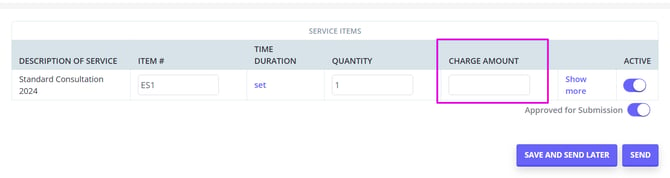
2030: Charge Amount must only be set when Service Type Code is set to G (Dental), L (Optical), I (Speech Pathology), J (Allied) or K (Psych). Error located in Medical Event {m}, Service {s}.
For the DVA community nursing service type, the claim Charge Amount should be left blank when submitting the claim:
2030: Referral Override Code must only be set when Service Type Code is set to G (Dental), L (Optical), I (Speech Pathology) or J (Allied). Error located in Medical Event {m}.
When this error notification is returned, it means that a referral is required for this type of claim. Please add the referral in Client Profile > Referrals.
2030 : Charge Amount must not be set if Distance Kilometers is set. Error located in Medical Event 01 Service C002."
To resolve this issue, enter data in either the 'Charge Amount' field or the 'Distance Kilometres' field for the travel service or line item—but not both. Setting values in both fields for the same line item will result in an error.
159: Item associated with other service which is payable.
This usually means you cannot claim for this service until another item number has been claimed. You may need to contact DVA to determine what item needs to be claimed.
532: GST details incomplete. Phone GST Team on 1800 653 629.
This error usually comes up when you have GST incorrectly applied to the service you're trying to claim with DVA. Most DVA services do not incur GST and will be Tax Exempt, and you will see this error if GST is applied when you try to submit the claim. Please go to Settings > Billing > Services and update your service's Tax Rate to Tax Exempt, Save, then resubmit the claim with the updated tax settings.
Please note you do not need to contact DVA in most cases if you're receiving this error.